Scientific Abstract
Background: Functional integration and segregation are the two guiding principles in human brain functional mapping. These two principles reflect the integrated and distributed nature of neuronal processing and brain organization. In brain imaging studies with fMRI, functional integration and segregation are indicated by the correlation and anticorrelation of the time course of spontaneous blood oxygen level-dependent (BOLD) signal, respectively. To date, most research has focused on functional integration, with less attention paid to the role of functional segregation. It is unclear whether functional segregation is a global impairment or only between certain brain regions. It is also unclear whether various psychotic symptoms with different neuropathological substrates are related to functional segregation impairments in different circuits. Moreover, there is considerable biological and clinical heterogeneity across psychosis syndromes. Conventional approaches investigating treatment outcomes based on clinical categorization and diagnoses are difficult to capture fundamental underlying neurobiological mechanisms of dysfunction and can be recall or responder biased. Thus, an objective neuroimaging biomarker for classifying patients and tracking the changes of psychotic symptoms would be crucial.
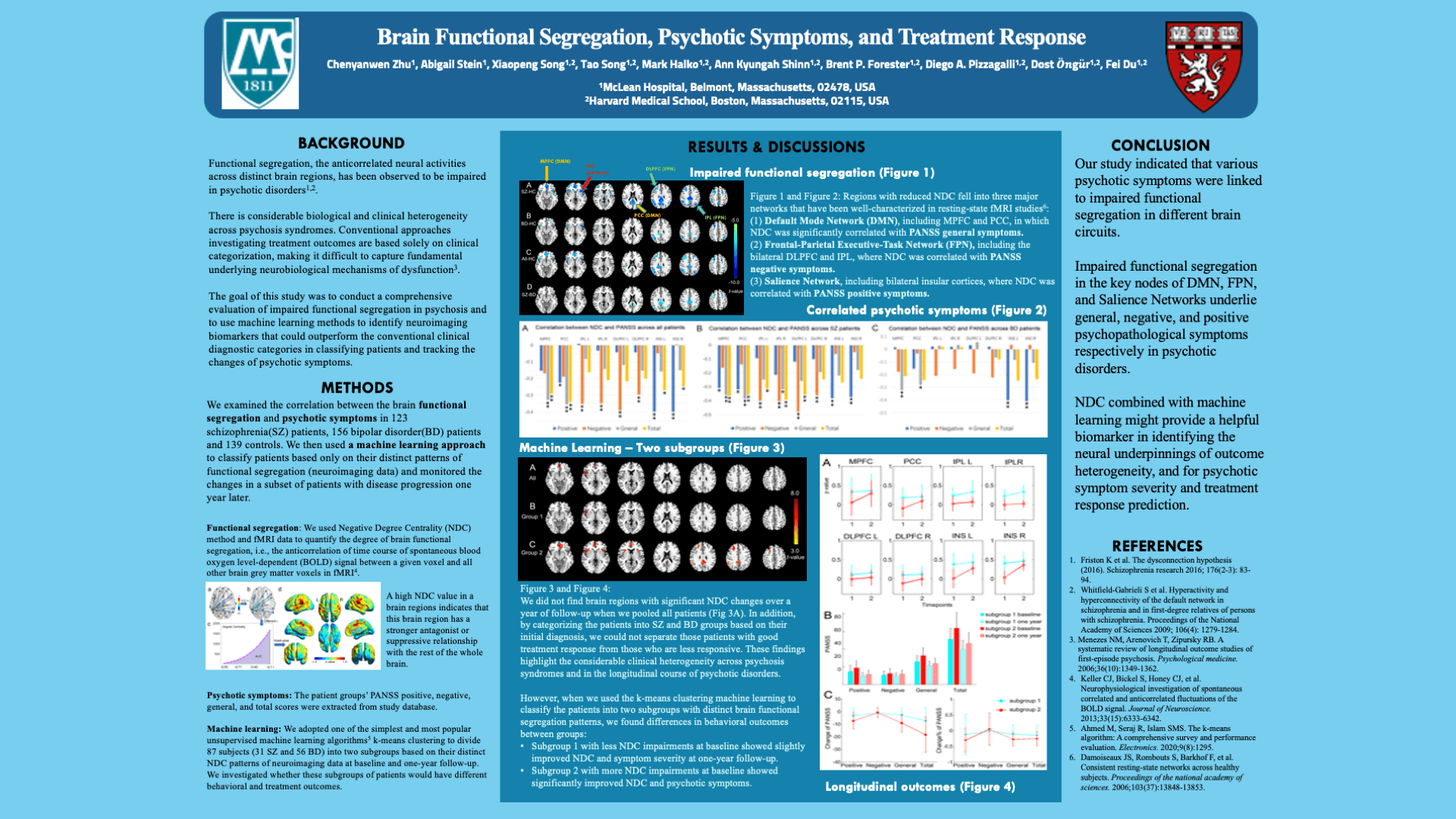
Methods: To address the above issues, we introduce the Negative Degree Centrality (NDC) method to quantify the degree of functional segregation between a specific region and all the other parts of the brain. A whole-brain data-driven analysis was applied for a comprehensive evaluation of impaired functional segregation in psychosis. We examined the difference of NDC among early-phase patients with schizophrenia (SZ, N=123), bipolar disorder (BD, N=156), and healthy controls (HC, N=139); and monitored NDC changes in a subset of patients (31 SZ and 56 BD) with disease progression one year later. We adopted an unsupervised machine learning classifier to subdivide patients based on distinct NDC patterns of neuroimaging data at baseline and one-year follow-up and investigated whether these subgroups of patients would have different behavioral and treatment outcomes. We hypothesized that: 1) various psychotic symptoms will be associated with functional segregation impairments in different neural circuits; 2) the combination of functional segregation and a machine learning method will outperform traditional diagnostic categories in tracking psychotic symptom changes and predicting treatment outcomes.
Results: Compared to HC, both SZ and BD subjects showed significantly decreased NDC at baseline. Positive, negative, and general psychotic symptoms were correlated with impaired NDC in the salience, frontal-parietal, and DMN, respectively. Using a machine learning approach, we identified two transdiagnostic patient subgroups with distinct recovery trajectories: one subgroup with more NDC impairments at baseline showed significantly improved NDC and psychotic symptoms, however, the other subgroup with less NDC impairments at baseline showed only slightly improved NDC and symptom severity at one-year follow-up.
Conclusions: Our study indicated that various psychotic symptoms were linked to impaired functional segregation in different brain circuits. NDC combined with machine learning might provide a helpful biomarker in identifying the neural underpinnings of outcome heterogeneity, psychotic symptom severity and treatment response, which could not have been revealed by categorizing them based on conventional clinical diagnoses. Our approach may help to develop precision medicine and personalized interventions in psychiatry.
Search posters