Scientific Abstract
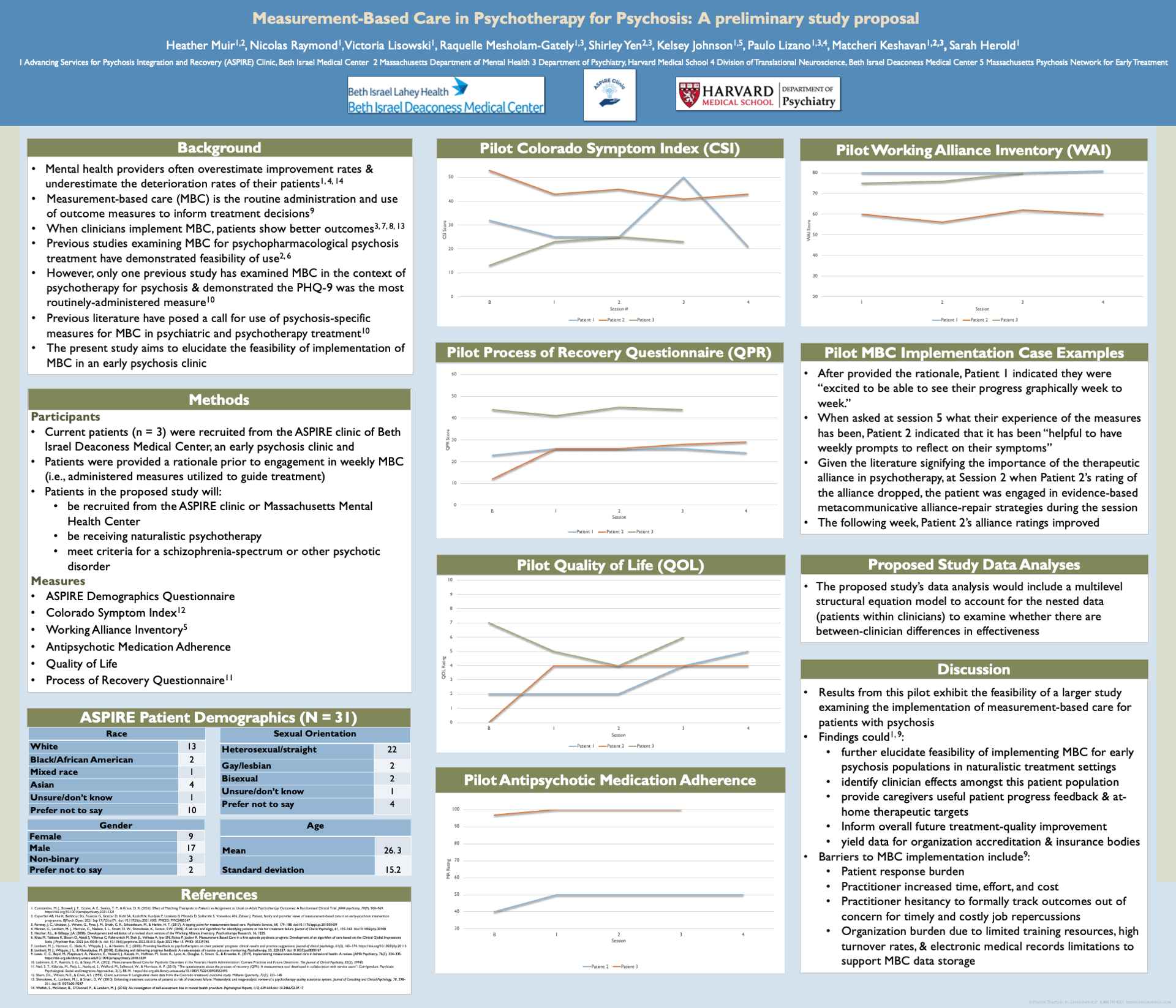
Background: Evidence suggests that mental health providers often overestimate the improvement rates of their patients and notably underestimate the deterioration rates for their caseload. Measurement-based care (MBC), the routine administration and use of outcome measures to inform treatment decisions, have been used to improve clinical decision-making and identify clinical strengths and weaknesses amongst clinicians. The benefits of using MBC for the average psychotherapy case have been established empirically by several systematic reviews and well-powered meta-analyses. However, only one MBC study has centered on psychosis patients, which demonstrated that the Patient Health Questionnaire-9 was the most routinely-administered measure. Thus, MBC in early psychosis programs is needed. The current proposal aims to elucidate the feasibility of implementing MBC for early psychosis patients, as well as determining whether therapist specific effects exist for this population.
Methods: Patients will be recruited from one of two study sites at Beth Israel Deaconess Medical Center or Massachusetts Mental Health Center, who are receiving naturalistic psychotherapy and meet criteria for a schizophrenia-spectrum or other psychotic disorder. Patients will be asked to complete a measure of psychosis symptomatology (i.e., Colorado Symptom Index), a measure of therapeutic alliance (i.e., Working Alliance Inventory), and a more general measure of distress (e.g., the Treatment Outcome Package) prior to each psychotherapy session.
Results: The nested data structure (patients within therapists) will be accounted for by using multilevel modeling to test whether there are between-clinician differences in effectiveness based on the Colorado Symptom Index and a global patient symptomatic/functional impairment index derived from the outcome tool.
Conclusions: Findings would elucidate the feasibility of implementing MBC for an early psychosis population in naturalistic treatment settings and identify whether clinician effects exist amongst this patient population. The findings from this study could inform future treatment-quality improvement.
Search posters