Scientific Abstract
Introduction: Polysubstance use has been linked to an increase severity in positive symptoms in psychosis; however, results on cognitive performance and structural neuroimaging measures are mixed. Here, we aimed to investigate lifetime polysubstance use on clinical symptoms, cognition and structural neuroimaging measures utilizing a large patient population from the Bipolar & Schizophrenia Network on Intermediate Phenotypes database.
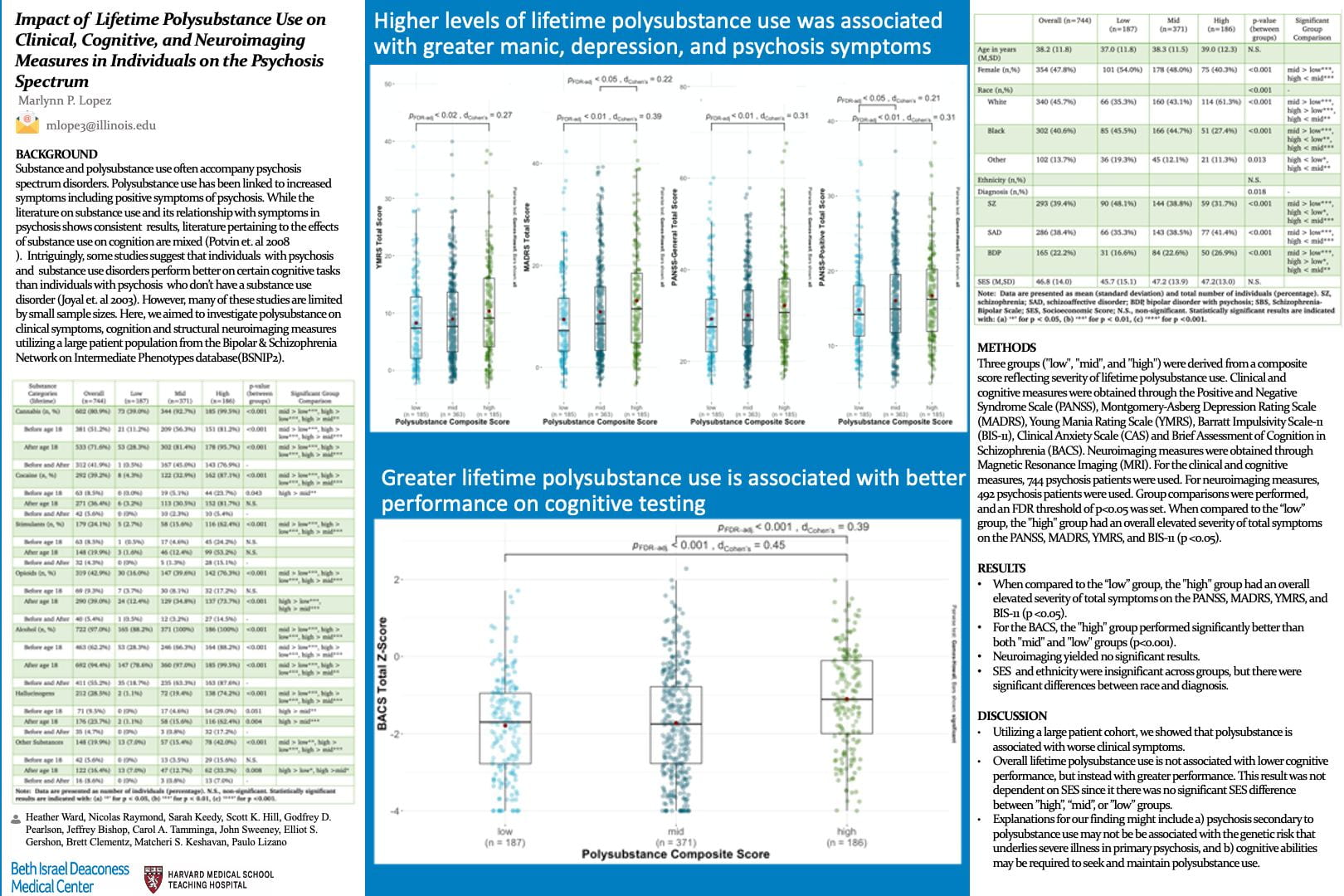
Methods: Three groups (“low”, “mid”, and “high”) were derived from a composite score reflecting severity of lifetime polysubstance use in 7 different categories: cannabis, stimulants, cocaine, alcohol, hallucinogens, opioids, and other substances. Clinical and cognitive measures were obtained through the Positive and Negative Syndrome Scale (PANSS), Montgomery-Asperg Depression Rating Scale (MADRS), Young Mania Rating Scale (YMRS), Barratt Impulsivity Scale-11 (BIS-11), Clinical Anxiety Scale (CAS) and Brief Assessment of Cognition in Schizophrenia (BACS). Neuroimaging measures were obtained through Magnetic Resonance Imaging (MRI). For the clinical and cognitive measures, 744 psychosis patients were used. For neuroimaging measures, 492 psychosis patients were used. Group comparisons were performed and an FDR threshold of p<0.05 was set.
Results: The “high” group had an overall elevated severity of total symptoms on the PANSS, MADRS, YMRS, and BIS-11 (p <0.05). In addition, the “high” group performed significantly better on the BACS than both “mid” and “low” groups (p <0.01). Neuroimaging findings were unremarkable across all groups.
Conclusion: Utilizing a large patient cohort, we showed that lifetime polysubstance is associated with severity of clinical symptoms. Our findings also indicate that higher cognitive performance may be a risk factor for greater polysubstance use in patients with psychosis.
Search posters