Scientific Abstract
Background: Studies following psychiatric patients from first episodes have helped to clarify diagnostic stability, treatment response, illness course and outcome. Most such research has focused on schizophrenia-like disorders, with very few studies of major affective and schizoaffective disorder patients followed prospectively over several years.
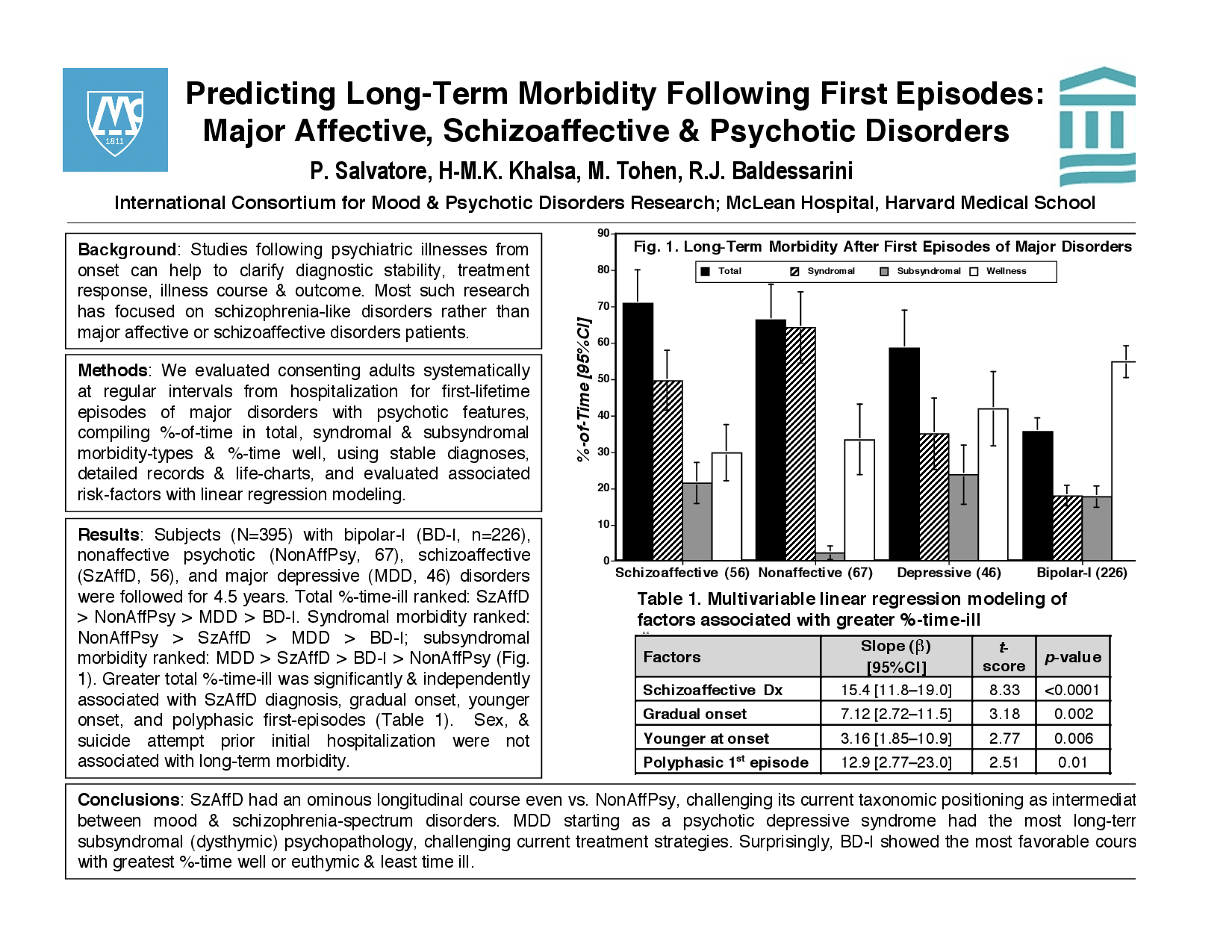
Methods: We evaluated consenting adults systematically at regular intervals from hospitalization for first-lifetime episodes of major affective, schizoaffective and nonaffective disorders with initial psychotic features. We compiled %-of-time in total, syndromal and subsyndromal morbidity-types as well as %-time well from detailed records and life-charts and compared those measures with stable diagnoses at two-years. We also evaluated associated risk-factors with linear regression modeling.
Results: Subjects (N=395) diagnosed reliably with bipolar-I (BD-I, n=226), nonaffective psychotic (NonAffPsy, 67), schizoaffective (SzAffD, 56), and major depressive (MDD, 46) disorders were followed for 4.5 years. Total %-of-time-ill ranked: SzAffD > NonAffPsy > MDD > BD-I. Syndromal morbidity ranked: NonAffPsy > SzAffD > MDD > BD-I, whereas subsyndromal morbidity ranked: MDD > SzAffD > BD-I > NonAffPsy. Greater long-term total %-time-ill was significantly and independently associated with SzAffD diagnosis, gradual onset, younger onset, and polyphasic first-episodes. Sex and suicide attempt as a reason for initial hospitalization were not associated with longitudinal morbidity.
Conclusions: SzAffD showed a particularly ominous longitudinal course even compared with NonAffPsy, challenging its current taxonomic positioning as intermediate between mood and schizophrenia-spectrum disorders. MDD starting as a psychotic depressive syndrome involved the most long-term subsyndromal (dysthymic) psychopathology, challenging current treatment strategies. Surprisingly, BD-I showed the most favorable course with greatest percent-time spent well or euthymic.
Search posters