Scientific Abstract
Background: Whole Health Systems (WHS) represents a paradigm shift in care for the Veterans Health Administration (VHA). WHS is a patient-driven approach to healthcare that focuses on Veterans’ values to guide goal setting and treatment. VA Boston Healthcare System has been a flagship site for WHS implementation. Within VA Boston, the Center for Returning Veterans (CRV) is a “first stop” mental health clinic for post 9/11 era Veterans. The goal of this project was to explore initial feasibility of implementing WHS elements into routine CRV care.
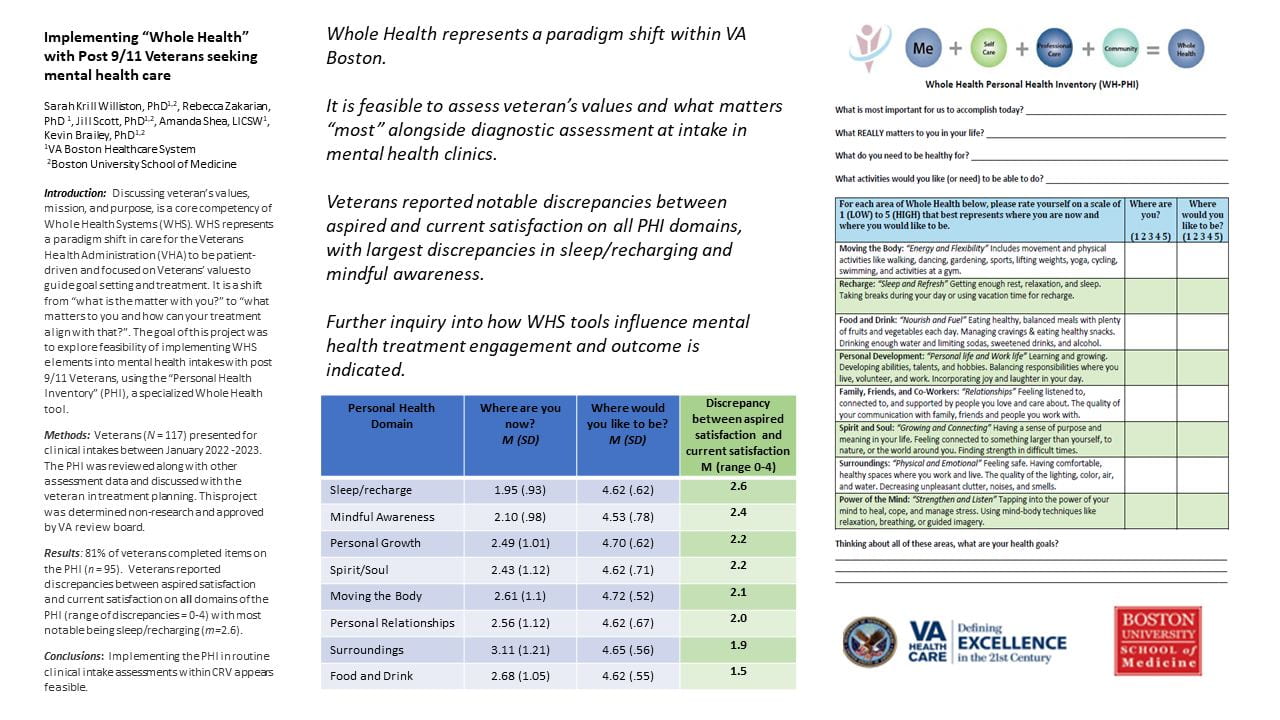
Our team incorporated the “Personal Health Inventory” (PHI), a specialized Whole Health tool, within a CRV program evaluation initiative. On the PHI, Veterans rate their relative satisfaction in life areas including: movement, nutrition, sleep/recharging, spirituality, relationships, physical surroundings, spirituality, mindful awareness, and personal growth on a 1 (low) to 5 (high) scale. The PHI also includes open response questions: “What matters most to you currently?” “What do you really need to be healthy for in your life?” Routine assessment and discussion of veteran’s values, including how those values guide treatment planning and goals, is a core competency of WHS approach.
Method: Veterans (N = 117) who presented for routine clinical intakes in the CRV between January 2022 and January 2023 were invited to complete clinical assessments, including the PHI, and semi-structured interviews. The PHI was reviewed along with other assessment data and discussed with the veteran in treatment planning discussions. This project was determined non-research and approved by VA review board.
Results: 81% of veterans completed items on the PHI at intake (n = 95). Veterans reported discrepancies between aspired and current satisfaction on all domains of the PHI (range of discrepancies = 0-4): sleep/recharging (m=2.6), mindful awareness (m=2.4), personal growth (m=2.2), spirituality (m=2.2), movement/exercise (m= 2.1), family/friend relationships (m=2.0), nutrition/diet (m=1.9), and physical surroundings (m=1.5).
Conclusions: Implementing the PHI in routine clinical intake assessments within CRV appears feasible. Further, veterans reported notable discrepancies in all areas of wellbeing, suggesting the Whole Health approach is important in this population. Further research examining how this tool works in treatment planning, such as fostering motivation, rapport, goal setting, and retention in care, will be important in future inquiry.